This Is Our Truth…
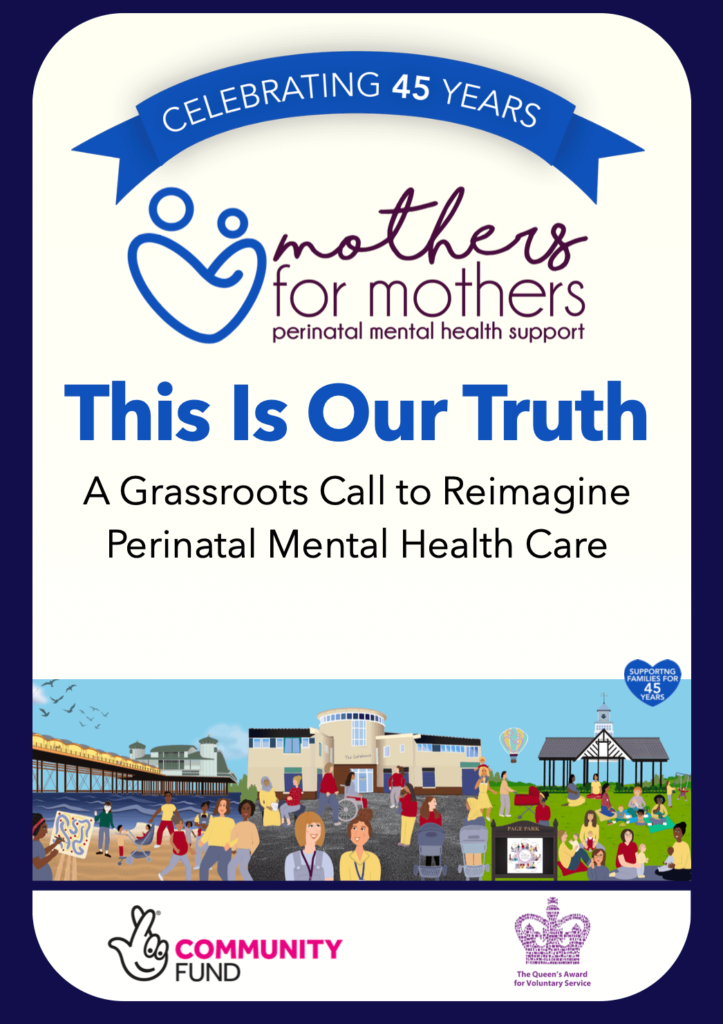
Yesterday, I was extremely privileged to be invited to an event INSIDE Parliament! Mothers for Mothers were celebrating their 45th birthday and the launch of their report: This Is Our Truth: A Grassroots Call to Reimagine Perinatal Mental Health Care. You might remember the adverts on here for it, or even have taken part in […]
This Is Our Truth… Read More »